Our medical billing services are supported by the Team’s deep industry expertise and technology we have to optimize your entire revenue cycle and take on your most time consuming tasks to ensure that your medical practice is running at maximum efficiency and profitability. Our team becomes an extension of your practice focused on your bottom line and reducing your administrative burden. Our advanced reporting and business analytics give you complete transparency and control of the entire billing process.
With Virtual Ops's Professional AR Management team, we are able to improve healthcare collections within a short period of time. Our success comes from accurate, timely and professional billing followed by serious A/R follow up, AR Clean Up and collections with dedicated AR professionals who use technology to process and accomplish the task of collecting more, faster.
Medicare, Medicaid and Commercial payers. We get you enrolled and we get it done right. Our services include full credentialing/enrollment, MAC setup and revalidation. We can quickly credential you with the necessary payors. Whether you are a solo practitioner or a multi-specialty group, that’s no problem!
Medical Billing Service is our center competency and we can proficiently deal with all you’re billing needs. Our medical billing experts have more than 18 years of involvement with all key protection payers including Medicare and Medicaid. Use the services of one of the top medical billing outsourcing companies to make your task less resource consuming.

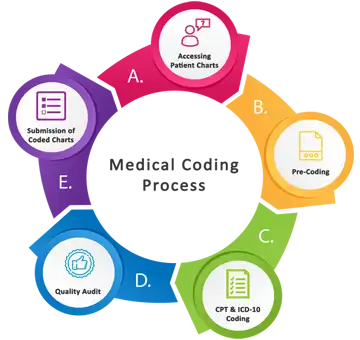
The patient list, a copy of the insurance card and demographic details are sent to us via email/fax or secure FTP. Our medical billing specialists call up the insurance company prior to the appointment. Pre-certification is done for specific lab tests, diagnostic tests and surgeries. The details are sent to the hospital/clinic in the prescribed format.
Our medical billing specialists enter patient demographic details such as name, date of birth, address, insurance details, medical history, guarantor etc as provided by the patients at the time of the visit. For established patients, we validate these details and necessary changes, if any, are done to the patient records on the practice management system.
The fee schedules are pre- loaded into the practice management system. CPT and ICD-10 codes are entered into the system. The billing specialists ensure that all details have been provided in the claim and ready to be filed.
Claims are submitted electronically via the practice management system. At this stage, a thorough quality check is done by a senior billing specialist and then submitted. The rejection report received from the clearing house, if any, is analyzed and the necessary changes are done. These claims are then resubmitted.
Scanned EOBs and checks are sent to our team for Payment Posting. All payments are entered into the system. The amounts from EOBs/checks and amounts posted in the system are reconciled on a daily basis. A daily log is updated with these data.
All claims in the system are examined and priorities are set. First the claims close to their filing limits, and then work down from the age of the claim. Periodic follow-ups over phone, email and/or online is done to get the status of each claim submitted to the insurance company. See our detail A/R Follow Service.
Denials Management including analysis of denials and partial payments is done by our senior medical billing specialists. Payors, patients, providers, facilities and any other participants are called to follow-up on denied, underpaid, pending and any other improperly processed claims and the action is documented in the system.
Virtual Ops is a Healthcare Revenue Cycle Management company focused on Insurance/Patient Collections.
We comply with HIPAA regulations and maintain high confidentiality of patient information. We sign NDA with every employee and audit on daily basis that none of the patient information goes out of our premises.
Credentialing or enrolling with government and commercial payers is challenging any way you slice it, but we’re here to eliminate the stress and increase the efficiency. As the first nationwide contracting and enrollment company, everyone else is still trying to play catch-up with our services and technology. We take care of everything from start to finish and keep you from spinning your wheels on the telephone for 4 hours a day. We offer physician credentialing services in all 50 states and work with thousands of providers every year. Our team of experts understands the insurance companies, and as former practice managers, we also understand what these insurance contracts mean to your bottom line. We provide contracting and insurance credentialing services to practices and hospitals of all shapes and sizes.
Provider credentialing is a time-consuming process where attention to detail is critical. Even the slightest error in the application process can cause it to be rejected, which would mean delayed or loss of revenue altogether. This is also the reason why Virtual Ops and our credentialing service exists today. We are here to bridge the gap between physicians and a payer’s network.
Physician credentialing services may assist individuals under the following scenarios:
Credentialing services are an absolute necessity for any physician or provider who wants to optimize the performance of their practice. Proper enrollment ensures that payment is not delayed or denied by the insurance carrier. After all, these scenarios often arise even if the physician is competent to provide his/her services to patients.
We are honored to mention that we are also providing Quality Medical Coding services at very reasonable rates. The Virtual Ops provides the quality medical coding services for physician groups, facilities and surgical centers allowing them to focus their attention on other concerns. Our staff consists of professional and qualified individuals, which are CPC and CPMA certified from AAPC and have profound experience in their field. Our exceptional professionals are well equipped with the knowledge and expertise, to get their job done efficiently. Our team of professionals and Innovative technology enables a workflow that minimizes errors, accelerates the billing process and reduces impact on your bottom line. We provide medical solution services including medical coding, medical auditing, and denial management.
At Virtual Ops our goal is to find a better way and for more than half a decade we’ve worked to build medical coding solutions that solve real coding problems, create real efficiencies and have a real impact on improving revenue and cash flow.
We provide accurate medical coding services at a cost-effective price, and can deliver the services our clients need. Our level of accuracy and fast turnaround time has set us apart from other medical coding outsourcing providers.
We provide medical coding services to facilities ranging from individual physician to major hospitals. Our staff has experience of providing coding services for almost every specialty and can handle tasks whether simple or complex efficiently, ensuring accurate coding with minimum errors.
Our Coding team has worked on multiple specialties and on multi-disciplinary requirements. Our Medical Coding. Auditing, Denial Management and consultation services can be used for all types of medical practices and medical specialties including:
Medical coding is the transformation of healthcare diagnosis, procedures, medical services, and equipment into universal medical alphanumeric codes. The diagnoses and procedure codes are taken from medical record documentation, such as transcription of physician's notes, laboratory and radiologic results, etc.
Backlog generally refers to an accumulation of works waiting to be done or orders to be fulfilled. Similarly, backlog coding refers to the coding of claims accumulated for a span of time.
Medical auditing entails conducting internal or external reviews of coding accuracy, policies, and procedures to ensure you are running an efficient and hopefully liability-free operation.
The goals of an audit are to provide efficient and better delivery of care and to improve the financial health of your medical provider. Medical record audits specifically target and evaluate procedural and diagnosis code selection as determined by physician documentation. Once areas of weakness are revealed through an audit, you can present the audit findings and identify opportunities for training in your health care organization.
Denial Management relates to management of claims which are denied by insurance companies due to incorrect billing or coding. Such claims are properly reviewed and then accurately coded to receive the proper reimbursement of the service provided. As, if such claims are not managed properly they result in heavy loss to the physician.
If you have big project at hand, and want find out more about our volume discounts contact us. Reduce costs and increase revenue and efficiency with our experts; contact us to get a free pricing quote.
Pricing Disclaimer
At Virtual Ops, we ensure that the information published on our website and our official documents are always accurate and current. We make sincere efforts to keep all the information accurate and up-to-date along with the pricing
Please note that all prices displayed on this official document are INDICATIVE, and final pricing is decided only after taking into the account various factors like nature of the project, complexity level, skill and experience of the resources, time required for completion and terms of contract. Prices displayed are subject to final approval at the time of order fulfillment, which could result in an increase or decrease in the price quoted on this document.